Is I am at risk of getting Prostate cancer or other cancer if my parent have cancer? Who can be screened for possibility or presence of Hereditary Prostate Cancer?
Is I am at risk of getting cancer if....................? Mostly children (sometime parents) ask this question. Today again. So, i tried to explain them that Usually NOT. About 10% of cases can be hereditary. Generally, if a person having some special pathology and risk factors then he is suspected for familial cancer.
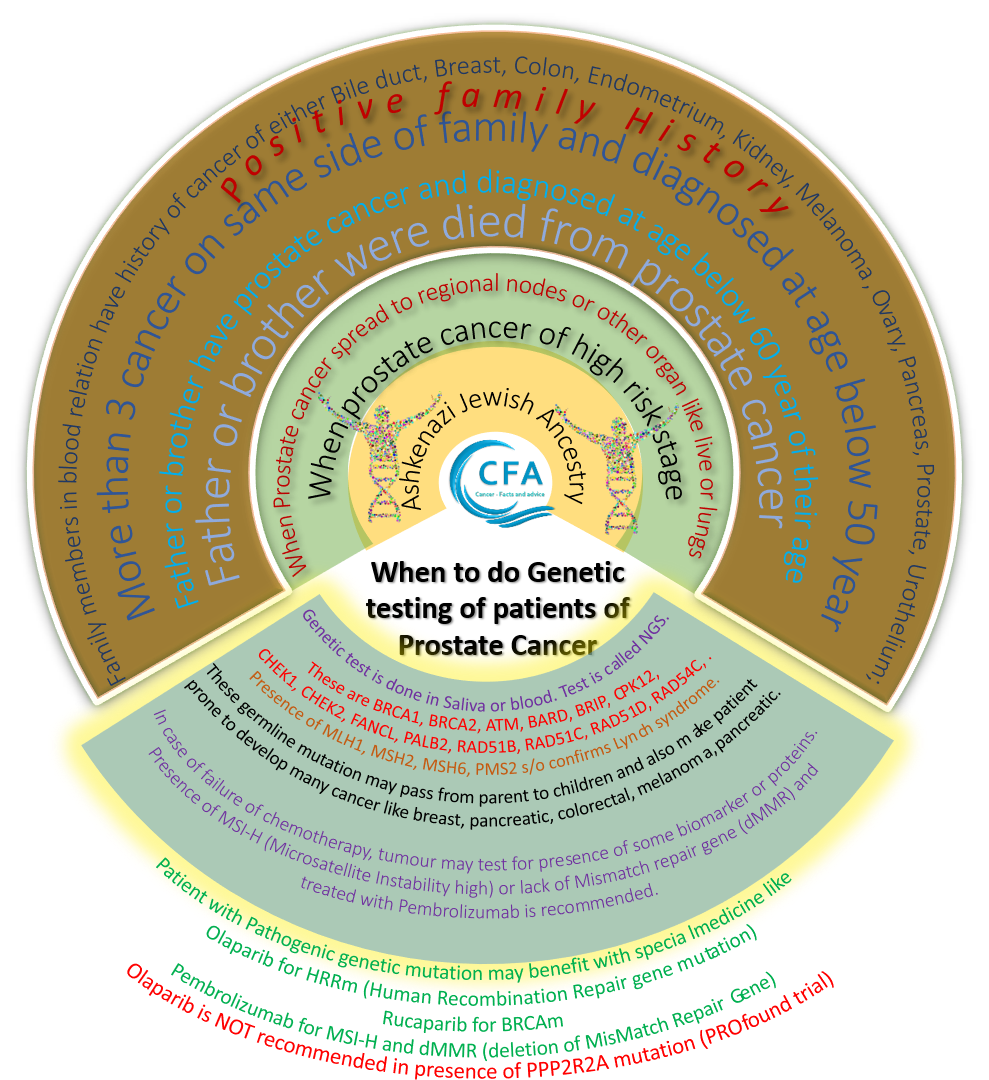
Risk factors for possibility of presence of genetic mutation are-
A. If your brother or father has been detected for high risk, advanced or metastatic prostate cancer at age below 60 year,
B. Biopsy is having intraductal or cribriform pattern,
C. If first degree relative died of Prostate Cancer.
Investigation for testing of presence of Genetic mutation-
If above, then send family member for counseling with "Genetic counselor". Based on case history and available facts, he may decide need of "Germline" or "Somatic" testing for presence of pathogenic mutation that are responsible for developing cancer. These genetic mutations are Lynch syndrome causing mutations or HRRm (Homologous Recombination Repair Gene Mutation). HRRm are BRCA1, BRCA2, ATM, BARD, BRIP, CPK12, CHEK1, CHEK2, FANCL, PALB2, RAD51B, RAD51C, RAD51D, RAD54C. Presence of MLH1, MSH2, MSH6, PMS2 confirms Lynch syndrome.
Mostly, these are associated with various cancers (e.g. Breast cancer, Bile duct cancer, Endometrial carcinoma, Ovarian cancer, Colon, Urothelial, Kidney, Melanoma,, Pancreatic cancer, Prostate cancer) having Ductal, intraductal or cribriform histopathology. They are helpful in planning of treatment if recommended routine treatment options failed. For example, Olaparib- in presence of HRRm, Rucaparib- in BRCAm and pembrolizumab- in MSI-H, dMMR.
Sometime, rare genes are also tested like HOXB13, PPP2P2A. It may helpful in treatment planning. Olaparib is not recommended in presence of PPP2R2A mutation. However, HOXB13 is associated with early age prostate cancer.
Testing of Germline mutation is done in blood or saliva. Test is called NGS (Next Generation Sequencing). Hundreds of pathogenic mutation are explored till today. They are either associated with development of different type of cancer or resistant to medicine or may cause progression. Thousands of mutation are detected but their role is unknown. Some of mutations are Drugable that means treatable. If these mutation happened in DNA then they may be carried by children. When these mutation get triggered by unknown factors they may produce cancer.
Genetic testing is recommended for patients with prostate cancer if they have-
1. Ashkenazi Jewish
2. Positive family history (means if father or brother or many family members are diagnosed to have high risk prostate cancer at young age (below 60 year of age) or diet of prostate cancer. Or, more than 3 types of cancers (Breast, Bile duct, Pancreatic, Gastric, Small intestine, Colon, Rectal, Kidney, Urothelial, Advanced Prostate, Endometrial, Ovarian, Melanoma) present in same side of family members (blood relation) who suffered before age of 50 years.
3. High risk or above (regional or metastatic) prostate cancer
4. Cribriform or Ductal / intraductal histology
Somatic testing-
In absence of valid recommendation for genetic testing, testing for "Somatic mutation" is done. These mutations are tested in tumour tissue and can be done by Immunohistochemistry (IHC) or NGS. It have potential to uncover genetic mutations but over-interpretation of possibility of genetic mutation should not be done. If anyone suspecting genetic mutation then it is better to do genetic mutation testing as no test is designed to do over-interpretation. Somatic testing may need to be repeated if cancer progress.
Somatic testing for HRRm can be considered if prostate cancer spread to regional node or metastatic; however MSI-H (Microsatellite instability - high) or dMMR (absence of Mismatch repair gene) are tested in metastatic CRPC (Castration resistant - Prostate cancer).


Comments
Post a Comment